Have you ever wondered how ageing affects your bones and muscles? Ageing and bone health, as well as ageing and muscle health, are critical topics that impact everyone's quality of life. The effects of ageing on bones often lead to conditions like osteoporosis, making bones brittle. Similarly, the effects of ageing on muscles include a decline in muscle mass and strength, leading to frailty and decreased mobility. Understanding these changes is crucial for effective joint care. By prioritising proper joint care, individuals can significantly improve their overall well-being and longevity and maintain an active, fulfilling life despite the natural ageing process.
What is Ageing and How Does It Impact Bones and Muscles?
Ageing is a natural and inevitable process that brings about a multitude of changes in the human body. While wisdom and experience are often associated with growing older, physiological transformations occur as we age, affecting various aspects of our health and well-being. Among these changes, alterations in bone density, muscle mass, and joint integrity stand out as critical factors with profound implications for our overall health and quality of life.
The human skeletal system supports our bodies and protects vital organs. Bones are dynamic structures that constantly undergo re-modelling throughout our lives. One of the most significant age-related changes in bones is a decline in bone density, primarily involving the loss of minerals such as calcium and phosphorus. This decrease in density contributes to osteoporosis, characterised by fragile bones vulnerable to fractures even with minimal trauma. Osteoporosis is a major public health concern among the elderly, leading to debilitating fractures, decreased mobility, and increased mortality rates.
In addition to changes in bone density, ageing affects muscle mass and function. The natural tendency to lose muscle mass, known as sarcopenia, impacts strength, balance, and physical performance. Sarcopenia involves a reduction in muscle fibres, increased fat infiltration within muscles, and a decline in muscle strength. These changes elevate the risk of falls, fractures, and disability in older adults. Maintaining muscle mass and function through resistance training, adequate protein intake, and lifestyle interventions is crucial for healthy ageing. (Novotny et al., 2015)
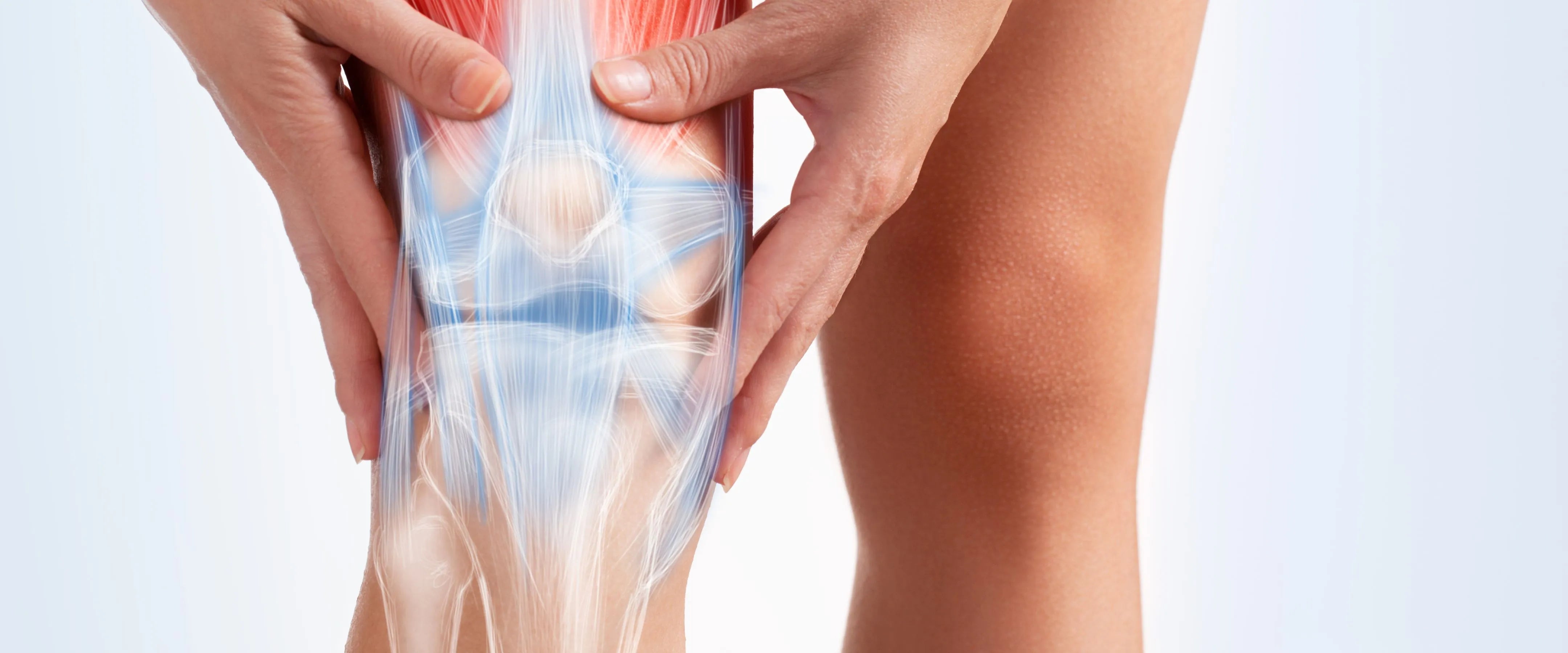
The Role of Bones and Muscles in Joint Health
The skeletal system, primarily composed of bones, forms the structural framework of our body, providing both stability and mobility. Bones connect at joints, supported by articular cartilage, ligaments, and bursae, enabling movement and flexibility. Besides movement, bones play critical roles in mineral storage and haematopoiesis, while muscles store carbohydrates as glycogen.
Joints, where bones meet, facilitate movement, and are classified into synovial (freely movable), fibrous (immovable), and cartilaginous (slightly movable) joints. Synovial joints, like the knee and shoulder, are lubricated by synovial fluid, reducing friction, and allowing a wide range of motions.
Bones and muscles work synergistically to support and move joints. Muscles, attached to bones by tendons, contract to pull on bones, generating movement. Ligaments and tendons provide additional stability, ensuring the integrity of joints during various activities. Changes in bone density and muscle mass significantly impact joint health. Decreased bone density can lead to fractures, while reduced muscle mass weakens support around joints, increasing the risk of joint pain and conditions like osteoarthritis.
Signs of Age-Related Joint Problems
Osteoarthritis (OA) is the most common joint disorder globally, and its prevalence increases with age. Studies have shown a significant rise in both radiographic and symptomatic OA among the elderly. For example, the Framingham Osteoarthritis Study found that the prevalence of radiographic knee OA increased from 33% in those aged 60-70 to 43.7% in those over 80. However, only a portion of these cases exhibit symptoms, highlighting the importance of combining clinical and radiographic criteria for an accurate diagnosis. (Anderson & Loeser, 2010)
Age-related joint problems, particularly OA, often begin with subtle symptoms that can be easily overlooked. Early signs of OA typically include:
| Early Signs of OA | Indicators Include |
| Stiffness | One of the first indicators is joint stiffness, especially after periods of inactivity or upon waking in the morning. |
| Pain | Persistent joint pain that worsens with activity and improves with rest is a common symptom. |
| Decreased Range of Motion | Difficulty moving the joint through its full range of motion can indicate early joint problems. This might manifest as a reduced ability to bend or straighten the joint fully. |
| Swelling and Tenderness | The affected joints may become swollen, tender to touch, and warm, indicating inflammation. |
| Grating Sensation | A grating or cracking sensation (crepitus) during joint movement is also a common early sign of OA. |
| When to Seek Help | Consult a healthcare professional if you experience any of the following |
| Persistent Pain | If joint pain persists for more than a few weeks and does not respond to over-the-counter pain medications or rest. |
| Significant Swelling | Noticeable swelling or tenderness in the joints that doesn't subside could indicate inflammation or other underlying issues. |
| Decreased Mobility | Difficulty performing daily activities due to reduced joint mobility should prompt a medical evaluation. |
| Joint Deformity | Visible changes in joint shape or alignment are serious symptoms that require immediate attention. |
| Impact on Quality of Life | If joint symptoms are affecting your ability to enjoy life, work, or engage in physical activities, seeking professional help is crucial. |
While older age is the greatest risk factor for OA, it is not an inevitable consequence of growing old. The relationship between ageing and OA is complex, involving changes within the joint tissues and other risk factors such as:
| Other risk factors | |
| Joint Injury | Previous injuries can increase the likelihood of developing OA in the affected joints. |
| Obesity | Excess body weight places additional stress on weight-bearing joints, contributing to OA development |
| Genetics | A family history of OA can increase one's risk of developing the condition. |
| Anatomical Factors | Abnormal joint mechanics, such as misalignment, can predispose certain joints to OA. |
Ageing affects joint tissues in several ways, increasing susceptibility to OA. Key ageing-related changes include:
| Ageing-related changes | |
| Cell Senescence | Ageing cells in the joint tissues adopt a senescent phenotype, secreting inflammatory molecules that contribute to joint degeneration. |
| Matrix Changes | The extracellular matrix of joint tissues undergoes alterations, including the formation of advanced glycation end-products, which impair the mechanical properties of the joint. |
| Oxidative Stress | Increased production of reactive oxygen species (ROS) with age leads to oxidative damage in joint tissues, promoting cartilage degradation and inflammation. |
Recognising the early signs of age-related joint problems and understanding the complex interplay between ageing and OA can help in managing and potentially slowing the progression of the disease. Timely consultation with healthcare professionals is crucial for early diagnosis and effective management, which can significantly improve the quality of life for those affected by OA. (Anderson & Loeser, 2010)
Preventative Measures and Joint Care Strategies
Healthy joints are vital for mobility and well-being, particularly as we age. Here are key strategies to promote joint health and prevent issues.
Lifestyle Modifications
- Engage in regular exercise: Incorporate low-impact activities such as swimming, cycling, or walking to promote joint flexibility and strength.
- Maintain a balanced diet: Consume foods rich in vitamins, minerals, and omega-3 fatty acids to support joint health. Include plenty of fruits, vegetables, lean proteins, and whole grains.
Longevity Supplements and Nutrition
- Fisetin: Enhances bone density by reducing inflammation and oxidative stress, promoting bone strength and health.
- Quercetin: Supports bone health by inhibiting bone breakdown and enhancing bone density through its antioxidant and anti-inflammatory properties.
- Ca-AKG: Provides essential calcium for bone strength while supporting energy metabolism crucial for bone formation and maintenance.
- NMN: Boosts bone health by activating sirtuins, promoting bone formation, and reducing age-related bone loss through cellular rejuvenation.
- Glucosamine and chondroitin: These supplements may help maintain cartilage health and reduce joint pain.
- Calcium and vitamin D: These nutrients are essential for bone health and can help prevent osteoporosis.
- Anti-inflammatory foods: Foods such as turmeric, ginger, and fatty fish can help reduce inflammation and alleviate joint discomfort.
Ergonomics and Posture
- Maintain proper posture: Sit and stand with your back straight, shoulders relaxed, and feet flat on the floor to reduce stress on joints.
- Use ergonomic furniture: Invest in chairs, keyboards, and desks designed to support proper posture and minimise strain on joints.
Recommended Exercises
- Stretching: Incorporate gentle stretching exercises to improve flexibility and range of motion in the joints.
- Strength training: Perform exercises targeting the muscles around the joints to provide support and stability.
- Low-impact cardio: Opt for activities like swimming, elliptical training, or cycling to increase heart rate without placing excessive stress on joints.
Benefits of Physical Therapy
- Customised treatment plans: Physical therapists can design exercises and techniques tailored to individual needs and goals.
- Pain management: Techniques such as massage, heat therapy, and ultrasound can help alleviate joint pain and stiffness.
- Improved mobility: Physical therapy can enhance joint function and range of motion, allowing individuals to maintain an active lifestyle.
Surgical Interventions
- Arthroscopy: Minimally invasive procedures to repair or remove damaged tissue within the joint.
- Joint replacement: Advanced techniques such as robotic-assisted surgery and personalised implants offer improved outcomes for joint replacement procedures.
- Rehabilitation: Post-surgical rehabilitation programs help patients regain strength, mobility, and function following joint surgery.
Real-Life Success Stories
Jitesh Kapadia (84, Retired Banker): Decode Age supplements impressed him! His weight is in check, and he has more energy, even in his 80s. Remarkably, his chronic pain has lessened, allowing him to keep dancing!
Conclusion
Prioritising your bone health and overall longevity is crucial for leading a fulfilling life. By taking proactive steps today, such as investing in Decode Age supplements for bone health or booking a consultation with our online Functional Medicine Health Advisory service, we pave the way for a healthier and more vibrant future. Your bones will thank you for it, and your future self will reap the benefits of your proactive choices. Let us embrace the opportunity to make informed choices and embark on a journey towards optimal well-being. Do not hesitate—seize the chance to invest in your health for a longer, happier life, starting now.
FAQs
How does ageing affect bone health?
With age, our bones weaken, increasing the susceptibility to fractures. Joint breakdown causes inflammation, pain, and stiffness, affecting posture, mobility, and energy levels. Muscle mass loss reduces strength and endurance over time.
Do we lose muscle as we age?
Yes, muscle loss begins gradually in our 30s or 40s, accelerating between 65 and 80. Rates vary, but up to 8% of muscle mass can be lost per decade. Factors such as physical inactivity, obesity, chronic diseases, and hormonal changes contribute.
At what age do bones stop regenerating?
Bones stop regenerating between 30 and 50 years of age. After peak bone mass, gradual bone loss occurs. Exercise, calcium, vitamin D, SeneVit, NNM and Ca-AKG intake are vital for minimising bone loss.
What are the effects of ageing on the muscles?
As we age, muscles shrink and weaken, leading to fatigue, weakness, and reduced exercise tolerance. Factors include reduced muscle fibres, slower tissue replacement, and changes in the nervous system affecting muscle tone and contraction.
What is joint care?
Joint care involves techniques to reduce strain and pain in daily activities, especially for those with arthritis. It includes modifying movements to protect joints, reducing inflammation, managing fatigue, and ensuring continued functionality.




















Leave a comment
All comments are moderated before being published.
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.