Gut dysbiosis is characterized by an alteration in the balance of the gut microbiota composition, with certain phyla becoming overrepresented while others are reduced in number. This leads to abnormalities within the gastrointestinal tract and the pathogenesis of commensal bacteria. Although most gut bacteria are beneficial, dysbiosis occurs when their population balance is disrupted, leading to mild and temporary symptoms that can progress to severe and chronic conditions if left untreated. Invasions by foreign microorganisms can destabilize the immune response and induce inflammation, which can facilitate the growth of pathogens and alter the balance of commensal bacteria. In this review, we will explore the relationship between the gut microbiome and chronic diseases, and the mechanisms that underlie this connection.
1. Introduction
The human digestive system contains a wide variety of bacteria that are constantly changing and have an important role in promoting and sustaining gut health. Traditionally, gut bacteria were regarded as incidental residents of the gut that only served as pathogens upon exiting the bowel. However, it is now widely accepted that the intestinal microbiota has a symbiotic relationship with the host and is essential in the development of chronic gastrointestinal disorders when present in abnormal concentrations or when located in gut regions that typically have low bacterial levels (1).
The gut microbiota is involved in a wide range of physiological processes, including metabolic activities, nutrient absorption, protection of mucosal surfaces, and immune system structure and function. Various factors, such as host age, genetic and environmental factors, diet, and exposure to drugs, including antibiotics and probiotics, influence the composition of the microbiota. The use of antibiotics can have a significant impact on the composition of the gut microbiota, with potential long-lasting consequences, especially for strains of bacteria that are resistant to antibiotics.
This alteration in the gut microbiota can create an opportunity for the development of superinfections caused by antibiotic-resistant bacteria such as Clostridium difficile or vancomycin-resistant Enterococcus. By utilising metagenomics methods, we have the potential to broaden our understanding of the gut microbiota in health and disease, particularly considering the significant variations that exist among bacterial groups. Changes in the quality and quantity of the gut microbiota have been linked to chronic illnesses (2).
2. Development of Microbiome
The human gut microbiota is initially colonized during and after birth, mainly by microorganisms from the mother's vaginal microbiota. Infants delivered through cesarean section tend to have reduced numbers of microbes in the gut compared to those born vaginally (3). The fecal microbiota of vaginally born infants was dominated by Acinetobacter sp., Bifidobacterium sp., and Staphylococcus sp. On the contrary, the infant born by cesarean delivery conspicuously lacked Bifidobacterium but was abundant in Citrobacter sp., Escherichia coli and Clostridium difficile (4).
During the initial three years following birth, the composition of an infant's gut microbiota undergoes rapid transformations which are influenced by various external and internal factors. These factors include the surrounding environment, the kind of food consumed, and the pH level within the intestine, as well as the host's secretions and immune responses. The diet of an infant plays a vital role in shaping their gut microbiome, as breast milk provides a limited range of microorganisms but is abundant in genes that facilitate lactate utilization. As an infant moves away from solely relying on breast milk and transitions to solid foods, their ability to use plant-based glycans experiences a shift (5).
By the age of three, the gut microbiome composition resembles that of an adult, and it remains stable until old age, with Bacteroidetes- and Firmicutes-dominated microbial diversity. However, long-term dietary changes or repeated antibiotic usage can disrupt this stability. Throughout various stages of life, environmental changes can modulate the microbiome composition, which plays a crucial role in defining and contributing to the host's physiology. Aging is associated with a decrease in Firmicutes/Bacteroidetes ratio, and the gut mucosa and lumen damage due to aging can lead to dysbiosis, a state of altered gut homeostasis, contributing to frailty (6).
3. Factors Affecting Gut Microbiome
The human gut hosts a high density of microorganisms that make up the human microbiome, and the relationship between them is symbiotic. The human microbiome undergoes continuous adaptation in response to various host factors. This process involves the production of signaling molecules by the intestinal epithelial cells that influence the composition and structure of the colonized surfaces. These signaling molecules include mucus, antimicrobial peptides and immunoglobulin A, which have the ability to either promote or inhibit the growth of specific microbial species (7).
Although an individual's core microbiota typically remains relatively stable throughout adulthood, it can vary among individuals due to several factors, including their entero-type, lifestyle decisions such as dietary patterns and physical activity, and cultural behaviours. The gut microbiota composition is influenced by a variety of factors, including age, nutrition, hormonal imbalances, inherited genes, and underlying health conditions. The gut microbiota plays a crucial role in the host's digestion and nutrition by breaking down substances that cannot be digested and producing essential nutrients. While the diversity of gut microbes is primarily established during early life, it can be altered by factors such as illness, antibiotic use, and changes in dietary habits (8).
Cultural heritage:
The diversity and composition of microbiota can be influenced by geographic location and ethnicity. Studies have shown that microbial composition can differ not only between countries, but also among different ethnic groups within the same country.
In a study involving 34 healthy individuals from urban northern and western regions of India, as well as adjacent rural areas, it was found that the gut microbiota of these individuals consisted of 50 core operational taxonomic units, including Prevotella, Faecalibacterium, Megasphaera, Ruminococcus, Lactobacillus, and Roseburia. The gut microbiota could be categorized into two groups based on the absolute counts of Prevotella and Megasphaera. Moreover, there was a difference in the microbial alpha diversity between rural and urban individuals, with urban individuals displaying greater diversity (9).
Diet/Food:
The gut microbiome is essential for the breakdown and synthesis of nutrients and vitamins that are not absorbed in the small intestine. These undigested food components, enzymes, and mucus are fermented by the colonic microbiota, resulting in the production of various metabolites that can affect the host's metabolic phenotype and disease risk. Fermentation primarily occurs with undigested protein and carbohydrates, resulting in the production of metabolites such as SCFAs, branched-chain fatty acids, and gases. SCFAs are particularly important, as they play both local and systemic roles in regulating energy metabolism, lipid metabolism, and glucose/insulin regulation (10).
Diet is a significant factor that influences the composition and diversity of the gut microbiome. A varied and complex diet is associated with greater microbiome diversity, while a Western diet that is high in fat and low in fiber is linked to a decrease in bacterial diversity and beneficial microbiota. Consuming a monotonous diet may also negatively impact gut microbiota diversity and health (11).
Antibiotics:
Regular use of antibiotics can negatively affect the gut microbiota by reducing species diversity and altering metabolic activity. The non-selective eradication of both commensal and pathogenic bacteria can result in a reduction of ecological richness and diversity. Recurrent exposure to antibiotics may contribute to antibiotic resistance. Early childhood exposure to antibiotics has been linked to gastrointestinal, immunologic, and neurocognitive conditions. Observational studies suggest a link between antibiotic use and gastrointestinal infections, weight gain, inflammatory bowel disease, and colorectal cancer (12).
Exposure to pathogen:
Pathogenic microorganisms and their metabolites such as lipopolysaccharides (LPS), genotoxins etc. in the human body can lead to inflammation in the gastrointestinal tract, which further destabilizes the gut microbiome. This can result in the outgrowth of harmful bacteria, leading to dysbiosis. In addition, chronic inflammation and autoimmune disorders can also negatively impact the gut environment, causing a disturbance in the microbiota's habitat. The breakdown of gut lining and cells can disrupt the symbiotic relationship between the microbial species and host, ultimately affecting the abundance and diversity of the microbiome (13).
Physical activity:
Exercise can impact the gut microbiota and contribute to energy regulation. It promotes the development of beneficial bacteria and increases diversity, correlating with protein intake and creatine kinase levels (14).
Age:
The gut microbiota in humans develops during early life and its composition, diversity, and complexity are influenced by various factors such as gestational age, mode of delivery, feeding methods, weaning period, genetics, environment, diet, lifestyle, and gut physiology. The microbiota diversity increases with age and eventually stabilizes as an adult microbiota composition mainly dominated by Firmicutes, Bacteroidetes and Actinobacteria. However, in individuals older than 70 years, changes in nutrient absorption and immune activity weakness may affect the gut microbiota composition (15).
4. Gut Microbiome and Chronic Diseases
Chronic diseases are illnesses that persist over a long time and may have no known cure e.g., diabetes, heart disease, inflammatory bowel disease etc.
Research has demonstrated that the gut microbiome plays a significant role in the development and progression of chronic diseases. Imbalances in the gut microbiota can cause chronic inflammation, which is linked to many chronic diseases. Additionally, the gut microbiome is involved in regulating the immune system, which is crucial in preventing and managing chronic diseases.
Autoimmune diseases
Autoimmune diseases (AIDs) are not solely caused by genetic factors but also by environmental factors. Among these, an imbalanced gut microbiota has become a topic of significant interest. The gut microbiota's composition and function have been found to be altered in several autoimmune diseases e.g., Rheumatoid arthritis, type 1 diabetes etc.
Rheumatoid arthritis (RA):
It is an autoimmune inflammatory condition that primarily affects the joints. Researchers have identified the gut microbiome as a possible factor in the development of RA, as germ-free mice have demonstrated resistance to experimental arthritis (16). Alterations in the diversity and composition of the gut microbiota have been observed in individuals with RA, with increased levels of Prevotella species and Collinsella potentially contributing to the development of the disease. In contrast, the abundance of beneficial microbes like Faecalibacterium was reduced in RA patients (17).
Type 1 Diabetes (T1D):
T1D is a condition where the body's immune system mistakenly attacks and damages the insulin-producing beta cells in the pancreas. This results in insufficient insulin production, which can lead to high blood sugar levels and a range of related health problems. Research suggests that health and the development of T1D in both humans and animals (18,19).
Animal studies have shown that changing gut bacteria with antibiotics or altering lipid metabolism can increase the risk of T1DM-like disease (20). In humans, studies have found changes in gut bacteria in those with T1D, including an increase in Bacteroides species and a decrease in those that produce important substances called short chain fatty acids (SCFAs) e.g., Faecalibacterium prausnitzii (21).
Atopic eczema:
Atopic eczema is a chronic skin disorder that is most common in early childhood. The development of eczema has been linked to skin-barrier dysfunctions, immune dysregulation, and interactions between the environment, host, and microbes (22).
Research suggests that the gut microbiome in early life is associated with the age of onset, severity, and remission of atopic eczema (23). However, the relationship between gut microbiome diversity and eczema development is still unclear, as some studies have found an inverse relationship between gut diversity and eczema severity. Instead, the development of eczema may be driven by specific gut microbiome signatures and their interactions with the immune system and the host (24).
People with atopic eczema tend to have higher levels of certain bacteria like Clostridium difficile, Staphylococcus aureus, and Escherichia coli, while having lower levels of other beneficial bacteria such as Bacteroidetes, Bifidobacteria, and Bacteroides. This imbalance can contribute to the development of eczema by triggering inflammation and reducing anti-inflammatory substances in the body. The dysregulation of specific bacteria, such as Faecalibacterium prausnitzii, which is responsible for producing short-chain fatty acids, may be the root cause of these changes (24,25).
Gut inflammation disorder
Inflammatory bowel disease (IBD):
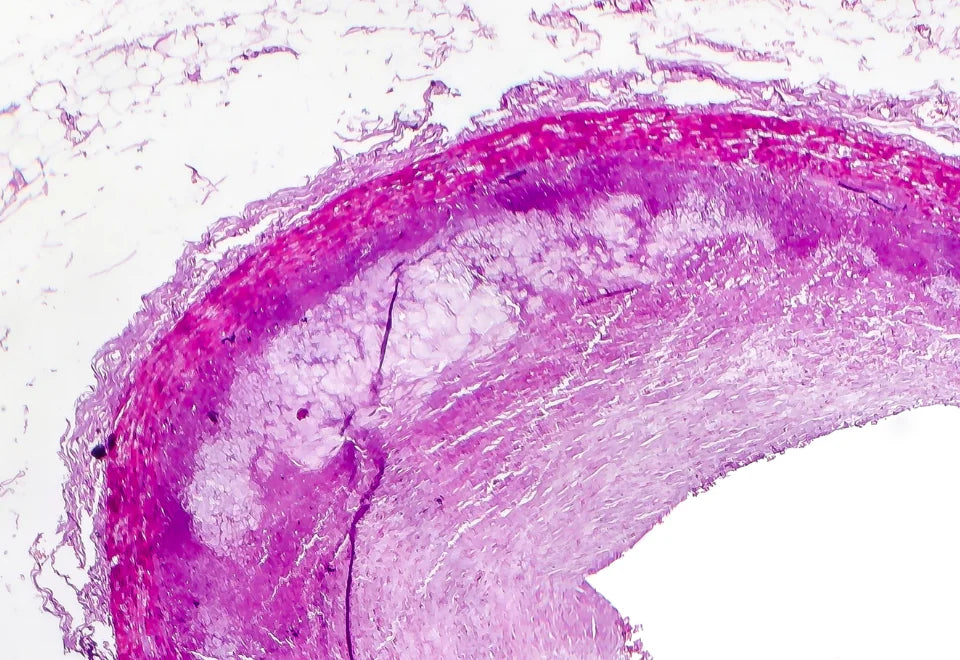
Inflammatory bowel disease (IBD) is a long-term inflammatory condition that affects different parts of the digestive system, leading to symptoms like abdominal pain, weight loss, rectal bleeding, and diarrhea. Ulcerative colitis is a form of IBD characterized by persistent inflammation in the large intestine, while Crohn's disease involves inflammation that reaches the deeper layers of the digestive tract. One important indicator of IBD progression is an increase in the ratio of Bacteroidetes to Firmicutes, with a decrease in the population of beneficial microbes like Faecalibacterium prausnitzii and an increase in opportunistic pathogens like E. coli and K. pneumoniae. These pathogens can activate the immune system and lead to chronic inflammation, which further affects the gut microbiota (26).
Irritable bowel syndrome (IBS):
Irritable bowel syndrome, also referred to as spastic colon, mucus colitis, or irritable colon, is a group of intestinal disorders that commonly manifest as abdominal pain, diarrhea, vomiting, and nausea. The exact causes of IBS are not fully understood, but there is a known correlation between dysbiosis and stress. In 2016, Nagao-Kitamoto et al., (27) reported that the patients with IBS had increased levels of Enterobacter and Veillonella species and decreased levels of Bifidobacterium and Lactobacilli species. Furthermore, bacterial members like Campylobacter, E. coli, and Shigella, as well as various fungal and viral parasites, have also been associated with the occurrence of IBS (28).
Cardiometabolic diseases
Cardiovascular disease (CVD):
Gut microbiota composition and metabolic potential have been identified as contributing factors in the development of CVD. Research has shown that dysbiosis, or an imbalance in gut microbiota, can contribute to the development of cardiovascular diseases. Specifically, studies have found a high level of proinflammatory bacteria in arteriosclerosis plaque, suggesting a pro-inflammatory effect that can contribute to plaque formation. Additionally, the conversion of choline to trimethylamine (TMA) by gut microbiota can lead to an increase in arterial plaques, which are associated with arteriosclerosis (29).
Gammaproteobacteria class has also been linked to endogenous alcohol production and non-alcoholic fatty liver disease, which in turn is associated with an increased risk of cardiovascular failure incidence. These findings suggest that the composition and function of gut microbiota may play an important role in the development and progression of cardiovascular diseases (30).
Type2 diabetes (T2D):
The gut microbiota of individuals with type 2 diabetes (T2D) has been found to differ from that of healthy individuals, but it is not yet clear whether these changes are a cause or a consequence of the disease.
Some bacterial genera, such as Bifidobacterium, Bacteroides, Faecalibacterium, Akkermansia, and Roseburia, have been found to be negatively associated with T2D meaning that higher levels of this type of bacteria may be linked to a lower risk of developing the disease. On the other hand, certain genera such as Ruminococcus, Fusobacterium, and Blautia have been found to be positively associated with T2D which means higher levels of this type of bacteria may be linked to a higher risk of developing the disease. This suggests that the presence of certain bacterial species in the gut microbiota may be linked to the development of T2D (31,32).
Moreover, studies have shown that individuals with T2D have lower levels of butyrate-producing bacteria and short-chain fatty acids (SCFAs), particularly butyrate, which has been linked to insulin sensitivity. Butyrate can stimulate the secretion of Glucagon-like peptide-1 (GLP-1) by intestinal L-cells via specific G protein receptors, which in turn can affect pancreatic function and insulin release, as well as central effects regulating appetite. Therefore, it is possible that the composition and function of gut microbiota may play a significant role in both the development and management of T2D (33).
Non-alcoholic fatty liver disease (NAFLD):
NAFLD and NASH (non-alcoholic steatohepatitis), which are increasingly common among people with obesity and type 2 diabetes, are thought to be strongly influenced by the interaction between the gut and liver, also known as the gut-liver axis. Gut dysbiosis, which is characterized by changes in the gut microbiome, is linked to increased intestinal permeability, which can cause damage to the intestinal barrier and lead to bacterial translocation. As a result, endotoxemia occurs, which can harm the liver through the portal vein (34).
According to research, there are consistent changes in the microbial composition of the gut of people having NAFLD. These changes are observed at different levels, including the phylum, family, and genus levels. Some of the changes include an increase in Proteobacteria at the phylum level and an increase in Enterobacteriaceae at the family level. At the genus level, there is an increase in the abundance of Collinsella sp, Escherichia, and Dorea, while there is a decrease in the abundance of Coprococcus, Eubacterium, Faecalibacterium, and Prevotella (35).
Research has found that certain bacteria such as Collinsella sp. can convert bile acids into oxo-bile acid intermediates. This conversion can cause an increase in intestinal permeability, which can contribute to the development of NAFLD. This increased permeability can also cause the release of lipopolysaccharide (LPS) into the host, leading to inflammation in tissues and the entire body. The metabolites produced by these bacteria, such as trimethylamine N-oxide (TMAO), choline, ethanol, and bile acid signaling, can also have an impact on the host's immune response (36).
Chronic kidney diseases (CKD)
The gut microbiota has been found to influence the gut-kidney axis in a reciprocal manner, with CKD altering the composition and functions of the gut microbiota, while the microbiota can manipulate processes leading to CKD onset and progression through various pathways. Studies have shown that individuals with CKD have altered gut microbiota, including decreased microbial richness, diversity, and uniformity. They also show lower levels of beneficial bacteria such as Bifidobacterium sp, Lactobacillaceae, Bacteroidaceae, Akkermansia and Prevotellaceae and higher levels of harmful bacteria such as Enterobacteriaceae (particularly Enterobacter, Klebsiella and Escherichia), as well as Enterococci and Clostridium perfringes (37).
One important probiotic, Akkermansia muciniphilla, is found at decreased levels in CKD patients and has been linked to chronic systemic inflammation, which is a major risk factor for CKD progression (38).
Neurodegentaive diseases:
The gut microbiota has been found to communicate with the brain through various pathways, collectively known as the "gut-brain axis," which includes the neural, immune, and endocrine pathways. This connection is crucial for the maintenance of mental health, and impaired functioning can lead to the manifestation of brain disorders.
Alzheimer disease (AD):
Alzheimer's disease (AD) development can be influenced by gut dysbiosis, which induces inflammation and immune dysregulation. The elderly population often experiences lower gut microbiota diversity and composition, which can lead to metabolic errors causing an imbalance in glucose levels, high circulating lipids, and increased levels of reactive oxygen and nitrogen species, all of which contribute to the pathophysiology of AD.
Proinflammatory bacteria like E. coli, Shigella, and Eubacterium rectale can affect the gut-brain axis, causing inflammation in the brain. Exposure of brain cells to lipopolysaccharide produced by B. fragilis can also lead to transcription of proinflammatory NF-ab p50/65 complex, resulting in neurodegeneration. Additionally, inflammatory bacterial amyloid proteins can cross-link with host amyloid, inducing misfolding and aggregation of neurodegenerative proteins like a-synuclein, Tau protein, and TDP43. A reduction in butyrate-producing bacteria can lead to increased levels of type 2 diabetes mellitus, which is a known risk factor for AD development (39).
Parkinson disease:
Parkinson's disease is a neurodegenerative disease, commonly seen in elderly people, characterized by symptoms like tremors, rigidity, and lack of coordination. The condition is associated with the accumulation of a protein called a-Synuclein in the brain and nerves. Recent studies have shown that the gut microbiome plays a role in the development of Parkinson's disease, likely via the vagus nerve, and constipation is a common early symptom. Additionally, the gut microbiome can affect the efficacy of the drug levodopa, which is commonly used to manage Parkinson's symptoms. This is because some gut bacteria produce enzymes that break down levodopa, reducing its effectiveness in the bloodstream of the patient (40).
Conclusion
The gut microbiome plays a primary role in maintaining host health, impacting metabolism, nutrition, physiology, and immune function. Dysbiosis of the gut microbiota is linked to various chronic diseases, including gastrointestinal conditions and wider systemic diseases such as metabolic syndrome, obesity, diabetes, cardiovascular disease and atopy. Bacterial metabolites, particularly SCFAs, appear to be the key agents involved. Butyrate-producing bacteria are associated with a lower risk of these diseases. Lifestyle and diet play a crucial role in maintaining microbiome diversity for healthy aging. Designing targeted dietary interventions to increase specific bacterial metabolites could provide a potential treatment strategy for these conditions.






















Leave a comment
All comments are moderated before being published.
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.