Did you know that more than half a billion people worldwide have diabetes?
Despite advancements in diabetes management and treatment, it remains a significant global health challenge, with approximately 1.5 million deaths directly attributed to the condition each year. Both the number of cases and the prevalence of diabetes have been steadily increasing over the past few decades, highlighting the importance of understanding different aspects of diabetes.
Diabetes is a metabolic disorder characterised by chronic high blood sugar levels. This condition arises from defects in insulin secretion, insulin action, or both, leading to metabolic abnormalities in carbohydrates, lipids, and proteins. Insulin plays a crucial role as an anabolic hormone, regulating the utilisation of nutrients for energy and growth. However, in diabetes, either the body produces insufficient insulin or the cells become resistant to its effects, particularly in skeletal muscles, adipose tissue, and the liver. The severity of symptoms depends on the type and duration of diabetes, with uncontrolled cases potentially leading to serious complications such as ketoacidosis or nonketotic hyperosmolar syndrome, which can result in stupor, coma, and even death. In this blog, we will take a comprehensive look at diabetes, exploring its various aspects in depth.
Differentiating Types of Diabetes
When it comes to managing diabetes, understanding the differences between types of diabetes is crucial. Let's get into Type 1 vs. Type 2 diabetes and other types as well as understand each type.
Type 1 vs. Type 2 diabetes
Let's discuss the differences between two common types of diabetes: Type 1 and Type 2 diabetes presented in a clear and concise table format. This will help clarify the key distinctions in their prevalence, causes, and diabetes management, providing a comprehensive overview of these prevalent forms of diabetes.
| Type 1 Diabetes (T1D) | Type 2 Diabetes (T2D) | |
| Otherwise called | Insulin-dependent diabetes or juvenile-onset diabetes | Non-insulin-dependent diabetes or adult-onset diabetes |
| Prevalence | ∼5-10% of cases | ∼90-95% of cases |
| Cause | Destruction of beta cells is caused by a cellular-mediated autoimmune response in the pancreas, leading to a lack of insulin production. | A combination of insulin resistance caused by the inability of the body to use insulin effectively. This results in relative insulin deficiency. |
| Treatment | Regular insulin injections or insulin replacement therapy | Lifestyle modifications along with oral medications or insulin therapy if necessary. |
| Prevention | - | Healthy lifestyle habits such as weight management, nutrient-dense diet and regular exercise |
Table 1: This table highlights the variances between Type 1 and Type 2 diabetes, focusing on prevalence, causes, treatment, and prevention strategies.
Other Types of Diabetes
Additionally, other types of diabetic conditions include prediabetes, gestational diabetes, and Maturity-Onset Diabetes of the Young (MODY), each with unique characteristics and considerations are explained in the table below:
| Prediabetes | Gestational Diabetes | Maturity-Onset Diabetes of the Young (MODY) | |
| Definition | A condition where blood sugar levels are higher than normal but lower as compared to type 2 diabetes. | Any degree of glucose intolerance detected during pregnancy. | The most common form of monogenic diabetes is characterised by autosomal-dominant inheritance. |
| Age of Onset | Mostly after 35 | During Pregnancy | Before 25 |
| Prevalence | ∼6.2% | ∼14.0% | ∼1% to 5% |
| Cause | Overweight or obese, family history of T2D, sedentary lifestyle | Hormonal changes, or high blood pressure during pregnancy and/or obesity | Mutation in genes that affect β-cell development or function |
| Treatment/ Management | Medication, healthy lifestyle choices | Medication or insulin therapy, healthy lifestyle choices | Medication, insulin therapy, or specific treatment depending on its subtypes |
| Prevention | Healthy lifestyle changes | Healthy lifestyle changes | - |
Table 2: This table outlines the distinctions among Prediabetes, Gestational Diabetes, and Maturity-Onset Diabetes of the Young (MODY) concerning age of onset, prevalence, cause, treatment/management, and prevention strategies.
Closer Look into Hyperglycaemia and Diabetes
The Glycemic Index (GI) is a valuable tool used to assess how quickly carbohydrate-containing foods raise blood glucose levels compared to standard carbohydrates. As different carbohydrates get digested and absorbed at different rates, it ranks foods on a scale from 1 to 100. This ranking helps categorise foods into three groups: low (1-55), medium (56-69), or high (70-100) GI. Understanding the GI of foods serves a great purpose in determining and managing blood sugar levels, particularly for individuals with diabetes. By choosing foods with a lower GI, one can avoid spikes in blood sugar.
But is there a direct correlation between glycemic index, and hyperglycemia, in diabetes development or management? Yes, there is a correlation between glycemic index, hyperglycemia, and diabetes. The glycemic index of foods affects blood sugar levels, and high-GI foods can lead to hyperglycemia, especially in diabetic patients.
Let’s first understand the concept of hyperglycemia before getting into this correlation. Hyperglycemia, often referred to as high blood sugar or high blood glucose, occurs when there is an excess of glucose in the bloodstream due to insufficient insulin production or insulin resistance. There are two primary types of hyperglycemia:
- Fasting hyperglycemia: This occurs when blood sugar levels are higher than 130 mg/dL after an 8-hour fasting period. If the fasting blood glucose falls between 100 mg/dL and 125 mg/dL, it indicates prediabetes, a precursor to diabetes.
- Postprandial hyperglycemia: This occurs when blood sugar levels exceed 180 mg/dL 2 hours after a meal. In individuals without diabetes, blood sugar levels rarely exceed 140 mg/dL after meals.
Studies have shown that limiting a high-GI diet reduces the risk of type 2 diabetes by 37% as this diet may cause pancreatic β-cell dysfunction, increase insulin resistance, and also lead to weight gain. The fasting blood glucose and insulin were significantly reduced by 30% upon consuming a low-GI diet. This diet along with high fibre content also resulted in improved postprandial hyperglycemia in the T2D patients. But, for effective results, you should take the carbohydrate content and energy intake into consideration.
Revealing Hidden Causes of High Blood Sugar
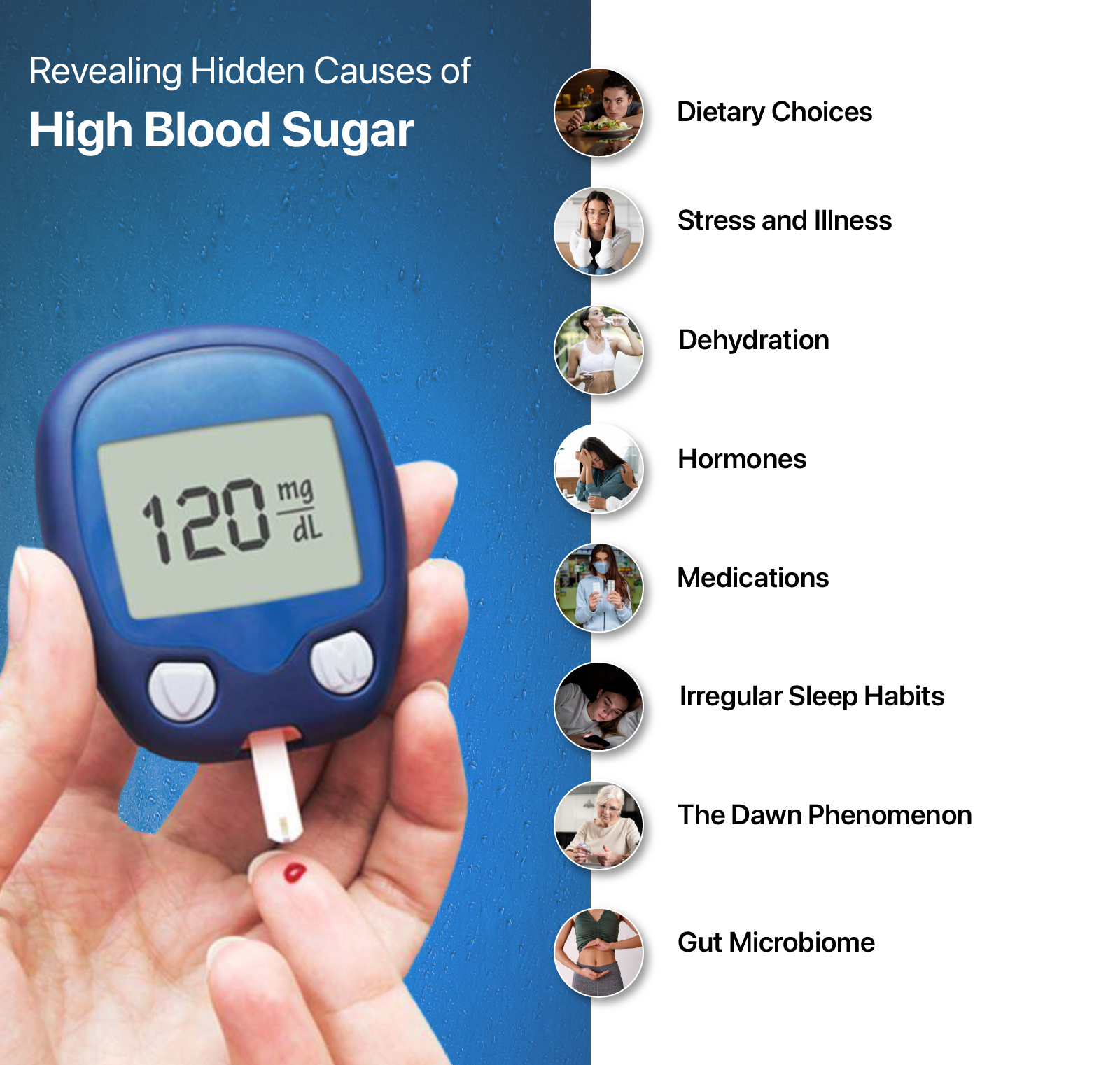
As we grasped the hyperglycemia being a concern in diabetes, let’s catch the culprits behind high blood sugar. Insulin resistance and pancreatic issues are the commonly known causes of hyperglycemia. So, we have listed down the hidden causes of high blood sugar below:
- Dietary choices: Processed foods and red meat elevate diabetes risk by 51% and 19% respectively. Added sugar can lead to blood sugar spikes, while high sodium intake can cause high blood pressure and heart disease. Sugary cereals, sweetened beverages and fruity drinks can quickly spike your blood sugar levels. These are some food choices that can catalyze hyperglycemia.
- Stress and Illness: Stress can be a hidden cause of hyperglycemia due to its impact on cortisol and pro-inflammatory cells like cytokines. Elevated cortisol levels, triggered by stress, promote glycogenolysis and gluconeogenesis, leading to an increase in blood sugar levels. Additionally, during times of illness, stress further exacerbates this effect, highlighting the importance of stress management in controlling blood sugar levels.
- Dehydration: It's surprising, but dehydration is one of the factors affecting diabetes control. When the body lacks adequate hydration, there's a shortage of water stores, leading to a higher concentration of glucose in the blood. This occurs as the body attempts to compensate for the fluid imbalance. Therefore, staying well-hydrated is not only important for overall health but also for maintaining balanced blood sugar levels.
- Hormones: Hormones such as insulin, and somatostatin are involved in blood glucose regulation, as well as insulin sensitivity can be a triggering cause. Ghrelin suppresses insulin secretion in islets or elevates blood glucose in diabetic patients. In women with type 1 diabetes, fluctuations in blood glucose levels can occur at different times during the menstrual cycle. During pregnancy, hormones from the placenta can lead to higher maternal blood sugar levels, as all pregnant women experience significant hormone shifts.
- Medications: Several medications can lead to elevated blood sugar levels. Steroids can interfere with insulin secretion from the pancreas, raising blood sugar levels. Mood stabilisers and some antidepressants can also affect blood glucose levels. Diuretics impair glucose metabolism and prolonged therapy can even lead to glucose intolerance. It's important for individuals taking these medications to monitor their blood sugar levels regularly and consult with their healthcare provider in case of sudden changes.
- Irregular sleep schedule: Lack of sleep or interrupted sleep patterns can lead to elevated blood sugar levels as it causes cells to respond poorly to insulin. Insulin resistance can result in a spike in blood sugar. Adequate sleep is essential for overall health, including the maintenance of balanced blood sugar levels.
- The Dawn phenomenon: Have you ever come across the Dawn phenomenon which is one of the factors affecting diabetes control? It is a common occurrence among people with diabetes, leading to high blood sugar levels in the early morning. Hormones like cortisol and growth hormone, naturally released in the morning, can increase blood sugar levels. This phenomenon highlights the importance of monitoring blood sugar levels and adjusting treatment plans accordingly.
- Gut Microbiome: The imbalance in gut bacteria is also a factor affecting diabetes control. In obese individuals, there is an increase in bacteria that produce butyrate, along with decreased glycine levels, which is linked to a higher risk of developing type 2 diabetes (T2D). Gut dysbiosis and leaky gut in obesity lead to the entry of pro-inflammatory molecules like lipopolysaccharide (LPS) into the bloodstream, triggering systemic inflammation. This inflammation contributes to insulin resistance and the progression of T2D.
Diabetes management can be complex, but adopting the right lifestyle habits can make a significant difference. You can make some key lifestyle changes for diabetes that can help take control of your diabetes.
Conclusion
Managing and treating diabetes requires a planned and supervised approach that addresses the various factors influencing blood sugar levels. For this, it’s quite important to understand the different types of diabetes, glycemic index, and hyperglycemia and address hidden causes of spikes in blood sugar. You can take control of your diabetes by adopting the above-mentioned healthy lifestyle habits and supplementation.
FAQs
What does type 2 diabetes mean?
Type 2 diabetes is the most commonly occurring diabetes, characterised by elevated blood glucose levels, also known as blood sugar. This condition develops when the body becomes resistant to insulin or is unable to use insulin effectively, leading to a relative deficiency in insulin.
What is the difference between Type 1 vs. Type 2 diabetes?
Type 1 and type 2 diabetes differ in their causes and how they affect the body. In type 1 diabetes, the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. As a result, the pancreas produces little to no insulin, leading to high blood sugar levels. On the other hand, in type 2 diabetes, the body becomes resistant to insulin or doesn't produce enough insulin to maintain normal blood sugar levels. This insulin resistance and relative insulin deficiency contribute to elevated blood sugar levels in the case of type 2 diabetes.
What blood sugar level is prediabetic?
Prediabetes is diagnosed when blood sugar levels are higher than normal but not high enough to be classified as type 2 diabetes. Specifically, a blood sugar level between 100 and 125 milligrams per deciliter (mg/dl) indicates prediabetes. It offers an opportunity to make lifestyle changes to prevent or delay the onset of type 2 diabetes.
What lifestyle leads to type 2 diabetes?
Type 2 diabetes is often linked to lifestyle factors such as obesity, physical inactivity, unhealthy diet, high-stress levels, and urban living. These factors can increase insulin resistance and lead to the development of type 2 diabetes.
What is the best way to manage diabetes?
The best way to manage diabetes is to understand the underlying causes and make informed lifestyle choices. This includes healthy eating choices, regular physical activity, monitoring blood sugar levels regularly, taking prescribed medications, stress management, and regular checkups.



























Leave a comment
All comments are moderated before being published.
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.