Have you ever wondered how the billions of bacteria in your digestive tract might be causing inflammation and pain in your joints? Our gut is home to a wide variety of microorganisms, and recent research shows that these microbes can play a big role in our health and overall wellbeing. One important association is between gut health and rheumatoid arthritis (RA), an autoimmune disease that induces joint pain and inflammation. In this blog, you will learn how rheumatoid arthritis may be affected by your gut microbiomes and what you can do about it.
What is rheumatoid arthritis?
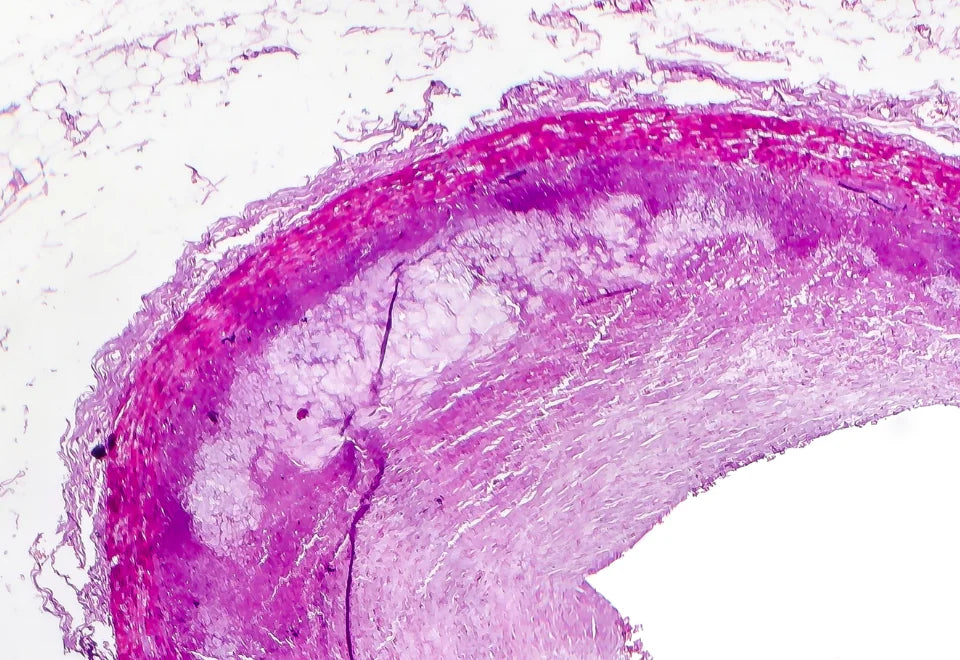
Rheumatoid arthritis is a chronic autoimmune condition that causes joint discomfort and inflammation. It occurs when the immune system, which fights and defends your body against infections, destroys its own healthy tissues in joints. The wrist, hand, elbow, shoulder, foot, spine, knee, and jaw joints could all be affected. Rheumatoid arthritis affects one in every 200 persons worldwide, with women having it two to three times more frequently than males (Smith & Berman, 2022).
Gut microbiomes and rheumatoid arthritis
The gut microbiota is vital for controlling our immune system. Gut dysbiosis, which is the imbalance of gut bacteria, has been associated with several autoimmune diseases including rheumatoid arthritis. Studies have shown that the gut microbiomes of people with rheumatoid arthritis are generally different from those of healthy people. The role of gut microbiomes in rheumatoid arthritis has been highlighted by numerous studies. The rheumatoid arthritis causes include the generation of proinflammatory metabolites, disruption of the intestinal mucosal barrier, and molecular mimicry of autoantigens (Zhao et al., 2022).
- Proinflammatory Metabolites: Gut dysbiosis makes substances that induce inflammation. This can cause immune cells to become overactive and produce more inflammation-causing chemicals (Zhao et al., 2022).
- Intestinal Barrier Dysfunction: The gut lining serves as a barrier, keeping potentially hazardous substances from entering the bloodstream. In rheumatoid arthritis, this barrier is compromised, letting harmful chemicals enter the bloodstream and triggering joint inflammation. Some gut microbiomes, such as Collinsella aerofaciens, can weaken the barrier, raising the risk of rheumatoid arthritis. Beneficial bacteria, such as Faecalibacterium prausnitzii, protect the barrier and minimise inflammation (Zhao et al., 2022).
- Molecular Mimicry: Sometimes, the proteins from gut microbiome can be similar to those in our own bodies. This similarity can fool the immune system and attack our own tissues causing rheumatoid arthritis (Zhao et al., 2022).
How does your diet affect arthritis?

What you eat affects the microbiome in your stomach. One important factor is the amount of fibre in your diet. We can't digest some dietary fibre; hence it needs to be broken down by gut microbiomes. Certain food choices can actually have an anti-inflammatory effect or a pro-inflammatory effect. Foods that trigger arthritis are:
Red Meat
Red meat contains saturated fats and substances like advanced glycation end products (AGEs) which increase inflammation and exacerbate arthritis symptoms.
Salty Foods
High-sodium foods, including bread and bread products, cheese and dairy products, and canned foods cause water retention, which increases the strain on joints, causing swelling and discomfort for arthritis patients.
Excessive Caloric Intake
Consuming too many calories can cause weight gain, ultimately putting pressure on the joints and worsening arthritis.
Added Sugar
Foods and beverages high in added sugar like cakes, cookies, white breads, soft drinks, fruit juices, and alcohol can spike inflammation in the body.
Vegetable Oils
Certain types of vegetable oils like sunflower, corn, and soybean oil can trigger arthritis.
Managing rheumatoid arthritis through gut health
Improving gut health may help decrease rheumatoid arthritis symptoms. According to research, having a healthy gut flora can minimise joint inflammation. A diet high in fibre, prebiotics, and probiotics can stimulate the growth of beneficial bacteria and lessen rheumatoid arthritis symptoms. Consuming fruits and vegetables rich in antioxidants, beans, whole grains, fatty fish, olive oil, nuts, and calcium-rich foods can all help in managing this condition. Supplements like vitamin D and omega-3 fatty acids may help regulate the immune response and also support a healthy gut environment in addition to dietary modifications.
Conclusion
The research into the link between gut health and rheumatoid arthritis is quite promising. Rheumatoid arthritis patients may discover new methods to symptom relief and quality of life by learning about and treating gut microbiome dysbiosis. As always, receiving personalised guidance and treatment alternatives from medical specialists is vital for properly managing rheumatoid arthritis.
FAQs
How serious is rheumatoid arthritis?
If rheumatoid arthritis is not treated or managed properly it can cause serious complications. It not only affects joints but also different parts of the body like the heart, lungs, kidneys, nerves and muscles. It can progress into moving problems. You may find it difficult to do your normal daily activities. This may lead to feelings of depression and anxiety. Additionally, it may increase your risk of infection, particularly if you are taking medication to treat the illness.
Can probiotics affect arthritis?
Probiotics are the live good bacteria which are beneficial for our gut. They help balance the gut microbiomes. It has been shown positive effect on rheumatoid arthritis. Since rheumatoid arthritis is an autoimmune disease indicated by chronic joint inflammation, improving gut health can possibly lower inflammation and ease symptoms.
Probiotics are helpful but they can not completely cure arthritis. They can be used as supplementary treatment in combination with medications and lifestyle changes. Always consult with your doctor before starting any medications.
Is yoghurt good for arthritis?
Yoghurt contains good bacteria called probiotics, which help improve gut health and inflammation. It is also a good source of calcium and vitamin D which is essential for bone health. People with arthritis have weakened bones and intake of yoghurt may ease the arthritis symptoms by reducing inflammation, which is closely linked with joint pain and stiffness.
What weakens the gut microbiome?
Many factors can weaken or damage the gut microbiome. Some of them are overuse of antibiotics, which kills the beneficial bacteria, along with the harmful bacteria in your stomach. Bad eating habits like intake of too much-processed foods, sugar, and unhealthy fats may cause gut dysbiosis. Immoderate alcohol consumption and smoking damage the gut lining and imbalanced gut microbiome. Poor sleep, long-term stress, and a sedentary lifestyle can also affect the gut health negatively. A balanced diet, stress reduction techniques, and healthy lifestyle decisions can all help to maintain a healthy gut microbiome.
Is arthritis curable?
There is no cure for arthritis, but if diagnosed early, it can be managed properly. Rheumatoid arthritis can be managed by medications, physical therapy, and lifestyle changes. In some cases, surgery may also be required, like joint replacement. Alternative methods like acupuncture, massage, and dietary supplements may provide additional relief for some individuals. The goal of the treatment is to improve the quality of life.
How can I reduce the risk of arthritis?
To avoid arthritis you can follow these strategies- do regular physical activities such as walking, cycling, and swimming for at least 30 minutes a day, maintain a healthy weight as excess weight can put pressure on your joints, eat plenty of fruits, vegetables, whole grains and foods rich in omega-3 fatty acids like fish and flaxseed, avoid alcohol and smoking, and get regular checkups.

























Leave a comment
All comments are moderated before being published.
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.