Have you ever wondered if signs of an unhealthy gut you are missing could be messing with your mood? If you suffer from gut dysbiosis or gut microbiome imbalance, your mental health might be more deeply affected than you realise.
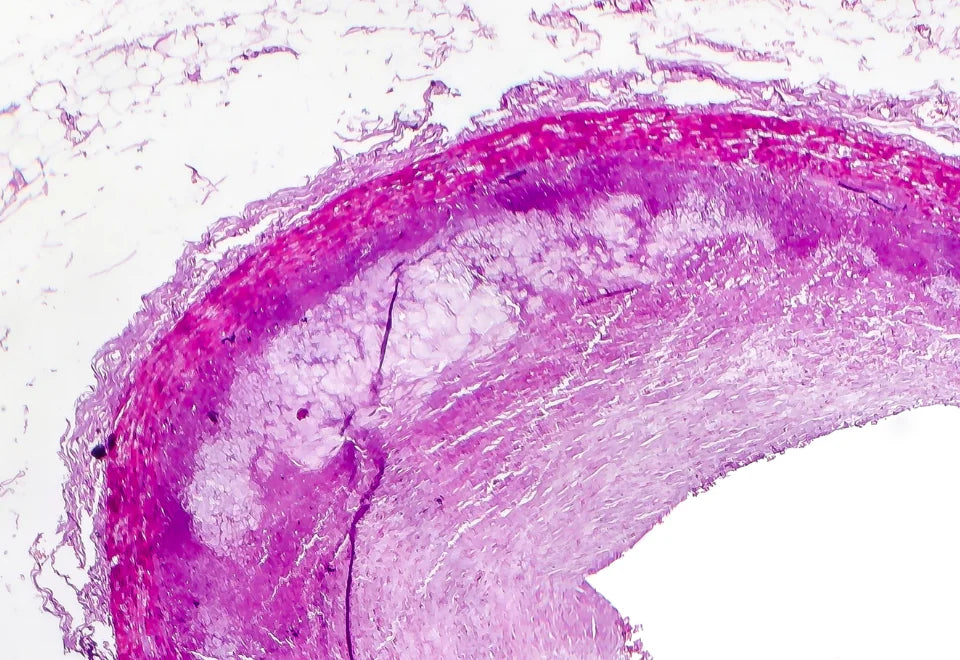
Gut dysbiosis refers to an imbalance in the gut microbiota, characterised by a disruption in the composition and function of the microbial community. This imbalance can lead to various health concerns, including digestive problems, immune system dysregulation, and even mental health disorders. When we particularly talk in terms of the brain-gut axis, a balanced microbiome supports stress resilience, while an imbalanced one can hamper mental health.
Dysbiosis can also lead to depression which can cause inflammation ultimately disrupting the gut biome. This intricate relationship highlights the significance of gut health and mental health. In this blog, we'll explore solutions for gut issues, aiming to restore harmony in the brain-gut connection.
Close-Knitted Brain-Gut Connection
The gut-brain axis serves as a complex communication network that integrates neural, hormonal, and immunological signals between the gut and the brain. This bidirectional system offers the intestinal microbiota and its metabolites a potential pathway to access the brain, suggesting a more accurate representation of the "microbiome-gut-brain axis." This axis plays a crucial role in influencing the development and function of the nervous system by modulating the gastrointestinal system, central nervous system (CNS), and immune system simultaneously (Mitrea et al., 2022).
One of the major nerves involved in this axis is the vagus nerve, which serves as a vital connection between the gut and the brain. It transmits signals in both directions, allowing for the transmission of information from the brain to the colon and back. This bidirectional communication is often experienced as a "gut feeling," highlighting the relationship between these organs.
This relationship has significant implications for mental health, brain disorders, and conditions such as irritable bowel syndrome (IBS), as stress can impact digestion, while digestive issues can affect mood.
The gut and brain are also interconnected through neurotransmitters, which are chemicals that control feelings and emotions. For instance, serotonin, a neurotransmitter that contributes to feelings of happiness and regulates the body clock, is primarily produced in the gut. Additionally, the gut microbiota produces neurotransmitters such as GABA, which helps control feelings of fear and anxiety.
The psychobiome is the community of microbes residing in the gut that influence our thoughts, feelings, and behaviours. They play a crucial role in converting dietary fibre into short-chain fatty acids (SCFAs). These SCFAs are sensed by the vagus nerve, which then sends signals to the brain to regulate digestion. This highlights the significant impact of gut health on brain function and mental health, emphasising the importance of maintaining a healthy gut microbiome for overall well-being.
Surprising Link Between Gut Biome and Mental Health
The bidirectional connection between the brain and the gut is crucial for overall health. This communication system highlights how the gut affects the brain and vice versa. The Enteric Nervous System (ENS), often referred to as the "second brain," spans the digestive tract and produces neurotransmitters that influence mood and sleep. Inflammation in the gut can lead to brain-related issues such as brain fog, depression, and anxiety.
Neural communication occurs with the help of the vagus nerve, neuropeptides, neurotransmitters and ENS, while humeral communication occurs through psychobiome, neurotransmitters, and SCFAs. Cytokines, hormones and metabolites are part of both communication systems.
Psychobiome plays a protective role in mental health, while others may contribute to the onset and progression of mental disorders. Studies have shown a clear dysbiosis of the gut microbiota in mental disorders such as depression, stress, eating disorders, psychotic episodes, and autism spectrum disorder (ASD).
This dysbiosis is characterised by a reduction in fermenting taxa and SCFAs concentrations, and an increase in opportunistic or pathogenic bacteria, contributing to a pro-inflammatory state.
In anxiety, social exclusion has been associated with increased Prevotella abundance and reduced Firmicutes: Bacteroidetes ratio and Faecalibacterium spp. levels. Depression is characterised by gut dysbiosis, with affected individuals showing differences in composition and abundance compared to healthy individuals. Bipolar disorder is marked by higher levels of Clostridiaceae, Collinsella, Actinobacteria, and Coriobacteria, but lower levels of Faecalibacterium and Ruminococcaceae. Schizophrenia, on the other hand, is also linked to dysbiosis, with unique gut bacteria found only in patients with the disorder (Xiong et al., 2023).
Leaky gut syndrome leads to the escape of toxins, and pathogens from the gut and triggers a chain reaction of detrimental effects. These substances activate the immune system, predominantly located in the gut. When immune cells sense a breach in the gut lining, they initiate inflammation. Chronic inflammation stemming from a leaky gut can lead to psychiatric symptoms. During periods of stress or inflammation, tryptophan, a precursor for serotonin production, can be diverted towards the kynurenine pathway. Prolonged activation of this pathway due to chronic inflammation may deplete serotonin levels and generate toxic substances in the brain, contributing to the neurotransmitter imbalances observed in anxiety and depression.
Moreover, gut microbiota can influence neurochemistry and neurologic function by modulating the metabolism of molecules related to enteric and central nervous system functions, such as GABA. This highlights the relationship between gut bacteria and mental health, emphasising the importance of addressing gut health in mental disorder management (Valle et al., 2023b).
Tummy Troubles Signalling Poor Gut Health Symptoms
While we previously discussed how an imbalance in the gut microbiome could extend to affect mental disorders, here we'll explore some common signs you might be experiencing because of your out-of-order gut health. Signs of an unhealthy gut microbiome can manifest in various visible ways like bloating, gas, diarrhoea, or constipation. However, specific signs may indicate an imbalance in gut bacteria and mental health, such as mood swings, anxiety, depression, or irritability.
1) Signs of Digestive Discomfort
Gas, bloating, and stomach issues can indicate an imbalance in gut bacteria, leading to poor digestion. These symptoms may be related to food intolerances rather than food allergies, affecting up to 20% of the population. While food allergies can cause severe reactions, food intolerances primarily result in discomfort and digestive problems.
When gut bacteria fail to properly break down certain foods, it can lead to gas and bloating after eating. This highlights the crucial role of gut health in digestive function and overall well-being, emphasising the importance of maintaining a balanced microbiome for optimal health.
2) Unexplained Weight Fluctuations
Sudden weight fluctuations can be one of the sneaky poor gut health symptoms influenced by gut health, as a balanced gut efficiently processes food and eliminates waste. However, certain gut bacteria can affect calorie extraction from food, impacting weight. Studies suggest a link between microbial richness and adult BMI, highlighting the role of the gut biome in weight management.
If you're experiencing unexplained weight changes despite stable eating habits, poor gut health and microbiome diversity may be contributing factors. It's essential to note that unintended weight loss or gain can also signal serious health conditions, such as cancer, underscoring the importance of consulting a healthcare professional if you experience significant weight changes.
3) Skin Troubles
Skin irritation can be linked to your gut health, particularly the balance of gut bacteria. Research suggests that consuming foods high in saturated fat and refined sugar can disrupt this balance, leading to a state of dysbiosis. This imbalance is associated with abnormal immune function, which can contribute to inflammatory skin conditions such as eczema, psoriasis, acne, rosacea, and dandruff.
Moreover, those with rosacea, red skin, often have more gastrointestinal issues, and a significant percentage of inflammatory bowel disease (IBD) patients also experience psoriasis, highlighting the gut-skin connection and the impact of gut health on skin health.
4) Emotional and Concentration Distress
Mental health issues can be influenced by gut health, as emotions are closely linked to the gastrointestinal (GI) tract. Anxiety and depression can lead to heightened brain activity, triggering similar responses in the gut. This cycle can exacerbate both psychological and GI symptoms, creating a feedback loop.
Addressing gut health through medications, lifestyle changes, and dietary modifications can help break this cycle and improve both GI and psychological symptoms
5) Energy Drain or Sleep Struggles
Struggling to sleep or experiencing excessive sleepiness could be linked to your gut health. The gut plays a significant role in serotonin production, a neurotransmitter that affects mood and sleep. Additionally, a disturbed sleep cycle can lead to chronic fatigue.
The relationship between sleep and gut health is bidirectional, as adequate sleep supports a healthy gut microbiome. Conversely, lack of sleep can lead to digestive issues, creating a cycle of poor gut health and sleep disturbances. It's crucial to address gut health to improve sleep quality and overall well-being.
6) Sweet Tooth Struggles
Excessive sugar cravings can be influenced by the types of microorganisms in your gut, as they may manipulate your eating behaviours to benefit your survival. This evolutionary conflict between the person and their gut microbes can lead to cravings for foods that promote the growth of sugar-loving microbes.
Instead of sugary beverages, opt for herbal teas or water infused with citrus fruit. Limit the intake of natural sweeteners while removing added sugars from your meals as the imbalance amount of nutritive sugar can disrupt the gut.
Reading nutrition labels can also help minimise consumption of hidden sugars in foods like condiments, and breads. These adjustments can help restore balance to your gut microbiome over time.

Scientifically Proven Tips for a Healthier Gut
Are you looking to improve your gut health and overall well-being? Your gut biome plays a crucial role in your health, affecting everything from digestion to mental health. While adopting a healthy lifestyle and dietary habits can positively impact your gut health, getting insights into your gut microbiome test can provide valuable insights based on various indicators of health. Here are some lifestyle and dietary habits that can help improve your gut health:
1. Your right choice of foods along with mindful eating habits can support a balanced gut microbiome. Even, focusing on a plant-based diet can promote a healthy gut and GABA neurotransmitter. Staying hydrated has also shown similar effects benefiting gut health.
2. You should engage in regular exercise as it increases the amount of good bacteria and the overall diversity of bacteria in the gut. You should aim for at least seven hours of uninterrupted sleep every night, as inadequate sleep can disrupt the gut microbiome and affect your food choices and mental health.
3. Smoking or alcohol intake and diets high in meat, sugar, saturated fat, and salt can promote pathogenic bacteria in the gut and also cause intestinal inflammation. You should quit smoking, or alcohol and reduce intake of these foods can restore balance in your gut.
4. When you’re experiencing stress, the body releases hormones such as cortisol that can negatively impact gut health. You should practise techniques such as meditation, walking or yoga as they can be beneficial in managing chronic stress levels.
Don’t worry! We've compiled a list of powerhouse foods that are beneficial for your gut and mental health:

1) Fibre: Fibre-rich diets including nuts, fruits, and vegetables help stimulate the diversity and growth of good bacteria in the gut. They also reduce oxidative stress, inflammation and stress hormones.

2) Probiotics: Probiotics found in fermented foods such as yoghurt, kefir, sauerkraut, and cheese help in soothing gut issues and reducing oxidative stress and inflammation. Psychobiotics also alter the brain activity.

3) Omega-3 Fats: Omega-3s found in salmon, flaxseeds, and fish oil can increase good bacteria in the gut. It supports increased memory and cognitive function. It also reduces the risk of neurodegenerative disorders.

4) Polyphenol-Rich Foods: Cocoa, green tea, olive oil, and coffee contain polyphenols that support the growth of healthy gut bacteria and improve cognitive function.

5) Tryptophan-Rich Foods: Tryptophan, found in foods like turkey, eggs, and cheese, is converted into serotonin, a neurotransmitter that can positively impact mood and gut health.

6) Vitamin D: Vitamin D-rich foods such as fortified foods, egg yolks, tuna, and salmon can be consumed to regulate the microbiome and reduce inflammation in the gastrointestinal tract.

7) Protein: Protein is found in sources like milk, yoghurt, and nuts beneficial for gut health and may also improve mood by promoting serotonin production.
Conclusion
You need to have a clear understanding of the gut-brain connection that highlights the profound impact of gut health on mental disorders. Also, recognising the signs of an unhealthy gut can lead to targeted interventions.
Stress management, regular physical activity, healthy dietary habits and quality sleep are vital for nurturing this delicate relationship. So, while you nourish your gut with healthy foods, remember to nurture your mind with positive habits to keep your brain and gut in sync for optimal health and well-being.
FAQs
Can an unhealthy gut affect your brain?
Yes, an unhealthy gut can affect your brain. Chronic inflammation triggered by gut issues lead to cognitive decline. Some gut microbes may negatively influence mental health, impacting neurochemistry and functions like memory and decision-making.
What are the signs of poor gut health?
Signs of poor gut health include digestive issues like gas and bloating, unexplained weight fluctuations, skin issues, emotional distress, fatigue, and sweet cravings. These symptoms indicate an imbalance in gut bacteria, affecting digestion, metabolism and mental health.
What foods help the gut-brain axis?
Foods that help maintain the gut-brain connection include fibre-rich foods, probiotics, omega-3 fats in salmon and flaxseeds, polyphenol-rich foods, tryptophan-rich foods, and vitamin D-rich foods. These foods help promote good gut bacteria, reduce inflammation, and support cognitive function.
What is the gut-brain connection called?
The gut-brain connection is called the gut-brain axis (GBA), which involves bidirectional communication between the central nervous system and the enteric nervous system, connecting emotional and cognitive brain centres with intestinal functions.
How to test gut health?
You can test gut health with microbiome testing kits like Decode Biome. You have to send your stool sample to a lab, and they'll provide a report detailing your gut microbiome composition and diversity.
Can a leaky gut cause mental illness?
Yes, a leaky gut can contribute to mental illness. It can lead to the escape of toxins and pathogens, triggering an immune response that can deplete serotonin levels and create toxic substances in the brain, potentially contributing to anxiety and depression.






















Leave a comment
All comments are moderated before being published.
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.